Lets start by breaking down the term ‘discogenic’. The disc is the structure that lies between the vertebrae, discogenic is pain that originates from this structure. Discogenic low back pain presents as pain in the lumbar spine with or without referral that is confirmed via X-ray, CT scan or MRI. Results are commonly reported as ” degenerative disc disease” or “multi-level disc degeneration”. This article aims to explain the role of the disc, what happens when they deteriorate and what it means for you if you have been diagnosed with disc disease or a disc herniation.
What is the disc?
The intervertebral discs are structures that lie between each vertebrae- vertebrae being the bony levels that make up your spine. Each disc contains a softer inner component called the nucleus pulposus and the outer component called the annulus fibrosis. The nucleus pulposus has a gelatinous centre with a water component of over 60%. The annulus fibrosis is made up of tightly packed connective tissue that encases the nucleus pulposus. There is a thin layer of cartilage above the nucleus pulposus that acts a barrier between the vertebrae above and below. This is the third component of the disc; the cartilaginous endplate. Anterior and posterior ligaments attach to the vertebrae to that provide additional reinforcement to the disc and resist opposing forces.
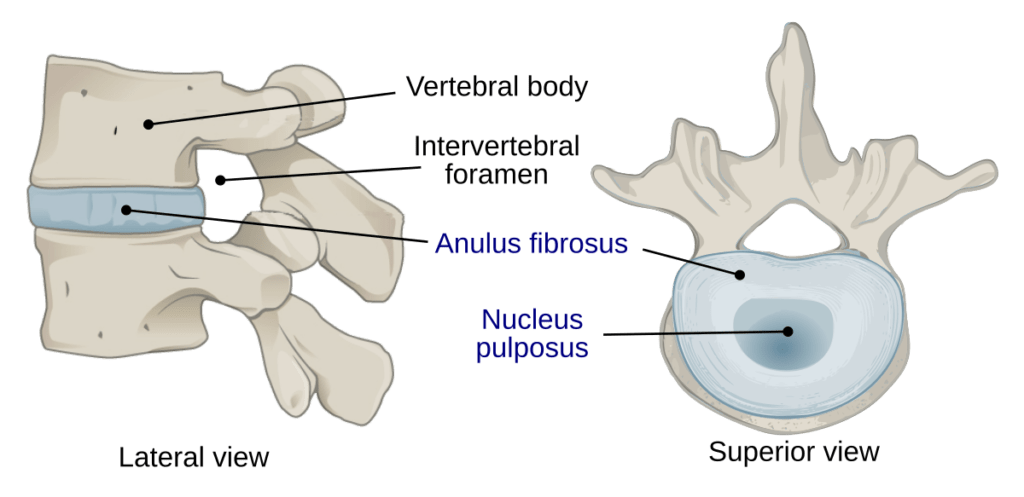
The disc provides height to the spine (25-30%), enables mobility, force transmission and prevents the vertebrae from moving directly on each other. The disc is thickest anteriorly in the cervical and lumbar spine relative to the curve (lordosis) present. When is comes to innervation and vascularisation it is excluded to the outer portion or the annulus fibrosis.
Disc degeneration
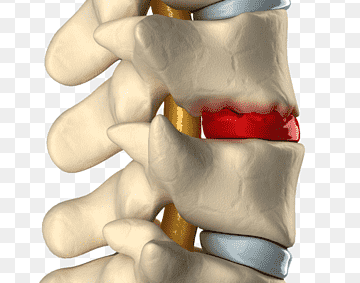
The disc undergoes a myriad of changes over time which alters the loading capacity. One of those is proteoglycan levels which have a direct relationship with water absorption into the nucleus pulposus. With a less hydrated disc there is less strength and increased response to spinal stress. Normal arterial supply is replaced by incongruous arterial segments which are smaller and subsequently impact on the nutrition of the disc. Varying concentrations of collagen sub-types impact the overall health of the disc and the susceptibility to mechanical stress. When the disc has undergone these structural changes, there is an impact on the capacity to distribute force/mechanical load. This moves the load towards the periphery and can increase the risk of herniation.
Disc Herniation
As the structure of the disc changes, there is an increased susceptibility to herniation or ‘bulge’. This is where the nucleus pulposus protrudes into the annulus fibrosis or the annulus fibrosis tears and facilitates this same migration of the nucleus pulposus. There are 3 different ways the disc can herniate:
- Protrusion: the disc bulges but doesn’t move beyond the vertebral end plate
- Extrusion: nucleus ruptures through the annulus but remains in one piece
- Sequestration: the nucleus ruptures through the annulus and fragments separate from the disc
Symptoms
Whilst most disc herniations will remain asymptomatic, those that extrude or bulge can irritate the surrounding nerve roots and cause changes in the periphery. Symptoms of a disc herniation can include: radicular pain, low back pain, changes to the sensorimotor nerve root distributions, limited range of motion and increased symptoms with coughing, sneezing or straining.
Your Physiotherapist or clinician through a detailed assessment will be able to then determine the level of the herniation. It is important to note, that a thorough subjective history will be taken prior to the physical assessment to screen for differential diagnoses.
Imaging
As stated in the definition of disc degeneration, diagnosis can only be confirmed via imaging but isn’t necessary unless symptoms persist beyond 12 weeks. This is largely due to the fact that not all disc herniations or degenerative changes result in pain or symptoms. Results found that over 50% of 30 year olds, 80% of 50 year olds and over 90% of 70 year olds have ‘Degenerative Disc Disease’ without any pain.
This supports our recognition that disc changes occur from adolescence and are in fact a normal part of the ageing process. Importantly, findings on imaging don’t correlate with the severity or location of symptoms in symptomatic individuals.
If your symptoms have persisted and are resulting in sensorimotor compromise, your clinician will refer you for a CT scan or an MRI which is the gold standard for detecting lumbar disc herniations. This is only the case if first line treatment and recommendations have failed, symptoms have worsened and progressed.
Management
Symptoms will often resolve within 6-12 weeks in 85-90% of the population with an acute disc herniation. When comparing conservative and surgical treatments, studies show outcomes are similar in the moderate and long term. Studies have shown that conservative intervention is better than no intervention for reducing both pain and disability.
Conservative treatment includes: movement/ physical exercise, education and reassurance in conjunction with pharmacological interventions. Your Physiotherapist is a great resource to provide exercises, activity modifications and utilise manual therapy when indicated.
Surgical options include discectomy, laminectomy or spinal fusions, all of which are a final option. As aforementioned, surgical outcomes in the long term are equivalent to conservative outcomes however when used for presentations of acute radicular symptoms, they can reduce symptoms and enhance quality of life in a shorter period of time.
References:
Al Qaraghli MI, De Jesus O. Lumbar Disc Herniation. [Updated 2022 Aug 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan.
Dydyk AM, Ngnitewe Massa R, Mesfin FB. Disc Herniation. [Updated 2022 Jan 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan.
Pourahmadi MR, Taghipour M, Ebrahimi Takamjani I, et al. Motor control exercise for symptomatic lumbar disc herniation: protocol for a systematic review and meta-analysis. BMJ Open 2016;6:e012426.