Posterior Tibialis Tendon Dysfunction (PTTD) is a common cause of medial ankle and foot pain affecting the tibialis posterior tendon, which – if not effectively treated – can have a detrimental impact on ankle/foot joint integrity and overall function. The severity of this condition can vary, as the tibialis posterior tendon can become inflamed and painful, or it can continue to deteriorate causing splits/tears within the tendon itself, leading to further complications within the ankle/foot complex. Therefore, identifying and treating this condition early can significantly improve patient outcomes and reduce the need for more radical interventions such as surgery.
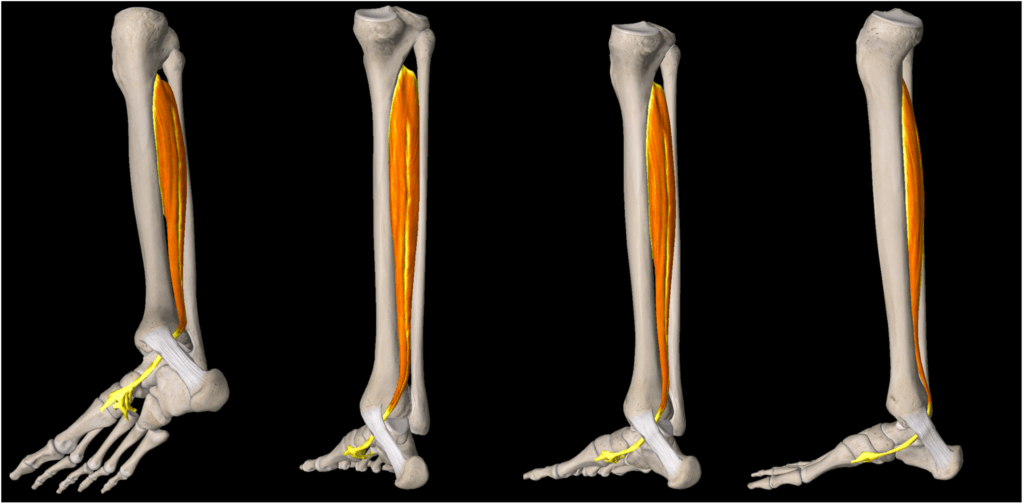
Anatomy of the Tibialis Posterior Tendon
The tibialis posterior tendon is one of the most important tendons within the ankle/foot complex. Originating from the tibialis posterior muscle belly in the calf region, the tibialis posterior tendon is situated posteriorly to the medial malleolus (inside ankle bone) and attaches itself to the navicular bone within the foot. The main function of this tendon is to lift the foot arch and support the foot when walking/running, but also has a role in ankle stability and foot/ankle kinetics.
Causes of PTTD
Research suggests the most common cause of PTTD relates to repetitive loading causing micro-trauma and progressive tendon degeneration. Other common causes relate to a history of ankle trauma either directly to the tendon or to the foot/ankle complex that can compromise normal foot biomechanics and potentially affecting how the tendon is loaded.
The tendon is susceptible to changes in foot posture and biomechanics due to its anatomical course, as it sits between ligaments/retinaculum and bones of the foot/ankle complex. Therefore, the tendon can be easily compressed or tensioned causing irritation and compromising its function. These postural changes within the foot can be caused by trauma (i.e., surgery or fractures) or congenital/degenerative changes (i.e., osteoarthritis or abnormal bony anatomy within the foot/ankle).
Common signs and symptoms
- Pain along the inside of the ankle with/without swelling
- Typically unilateral pain (rarely occurs bilaterally)
- History of trauma to the ankle or overload (increased running/walking activity)
- Aggravated by walking/running particularly on uneven surfaces
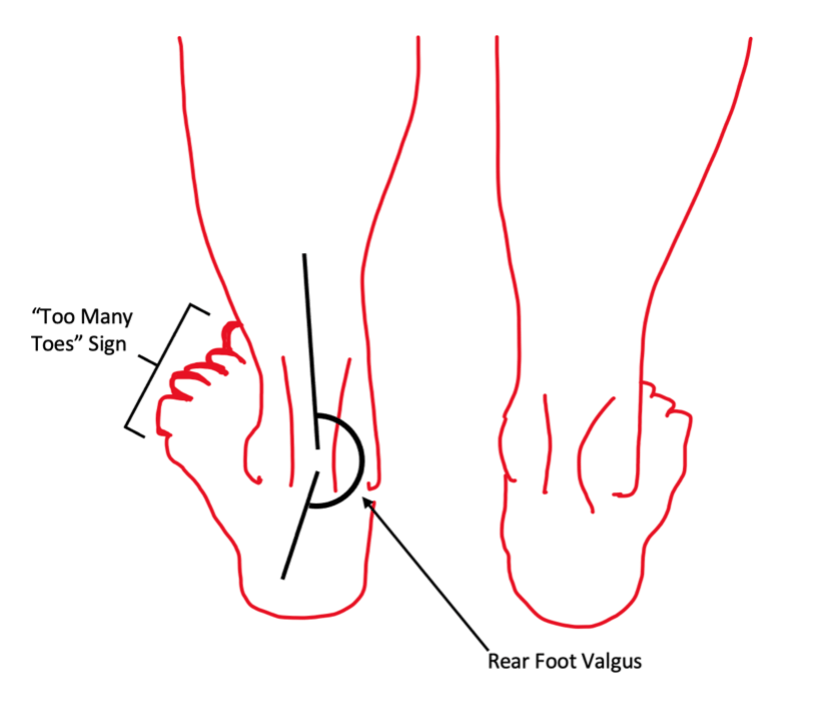
- Flat feet or “too many toes sign”
- Pain reproduced on single leg heel rise (sometimes double leg heel rise if irritable)
- Risk factors include being over 55 years old, hypertension, diabetes, and obesity

Licence link: https://creativecommons.org/licenses/by-sa/3.0/
Treatment of Posterior Tibialis Tendon Dysfunction
Management for this condition depends how severe the disease is. There are multiple ways to assess this condition and no one PTTD classification has been identified as superior as there are a lot of complex factors to consider, particularly if surgical intervention is needed. The commonality between all classifications determines the integrity of the tibialis posterior tendon and the main supporting joints within the foot and ankle complex that support normal foot/ankle mechanics.
One commonly used classification system is the Johnson and Strom classification. It considers several factors associated with PTTD and can guide treatment decisions for both conservative and surgical interventions. The Johnson and Strom classification system uses both clinical and radiological features to determine the stage of PTTD.
STAGE 1: Tenosynovitis +/- Reactive Tendinopathy without deformity
Clinical Features:
- Generalised pain (likely tenosynovitis) or localised pain (likely tendinopathy) with/without swelling
- Able to perform single heel rise with/without pain
- Potential weakness with ability to facilitate rearfoot varus movement with single leg heel rise
- No foot deformity
STAGE 2: Elongation and Tendon Degeneration (postural deformity)
Clinical Features:
- Flatfoot Deformity
- Flexible hindfoot
- Heel rise painful with/without ability to facilitate rearfoot varus movement
- Further categorisation
- IIA (Normal rear foot alignment)
- Negative “Too Many Toes” sign
- IIB (Postural rear foot valgus)
- Positive “Too Many Toes” sign
- IIA (Normal rear foot alignment)
STAGE 3: Elongation and Tendon Degeneration + Subtalar Arthritis (structural deformity)
Clinical Features:
- Flatfoot deformity
- Rigid hindfoot valgus
- Rigid forefoot ABd
- Unable to perform heel rise due to pain and/or stiffness
STAGE 4: Elongation and Tendon Degeneration + Subtalar Arthritis (structural deformity) + Valgus Tilt of Ankle Mortise (tibiotalar arthritis)
Clinical Features:
- As for Stage III with talar tilt in mortise
- Further categorisation
- IVA (Flexible)
- No fusion of ankle mortise
- IVB (Rigid)
- Fusion of the ankle mortise
- IVA (Flexible)
Conservative management is generally recommended for stages I and II, as the joint integrity is preserved. Research supports treatment options focusing on symptom management using load management principles, manual and ice therapy, discussing non-steroidal anti-inflammatories with appropriate health professionals, and various devices to assist with foot posture (i.e., CAM boot/strapping/orthotics). This is in conjunction with an appropriate exercise program to recondition the tibialis posterior tendon and maintain or improve the patient’s overall physical condition. Unfortunately, the overall amount of evidence identifying superior management/exercise techniques to improve the tibialis posterior tendon condition is limited. It should be noted that cortisone injections into the tibialis posterior tendon are contraindicated, as cortisone has a known catabolic effect on tissue. This will inevitably lead to further tendon degeneration.
If a patient is identified to have either a stage III or IV PTTD, or is not responding to conservative management, a specialist review should be considered to determine if a surgical intervention is appropriate.
References:
Abousayed, M.M., et al. Classifications in Brief: Johnson and Strom Classification of Adult-acquired Flatfoot Deformity. Clin Orthop Relat Res 474, 588–593 (2016).
Durrant, B., et al. (2015). Posterior Tibial Tendon Dysfunction: What does the single heel raise test mean in assessment? Foot and Ankle Online Journal, 8(2), 1-7.
Myerson MS, et al. Classification and Nomenclature: Progressive Collapsing Foot Deformity. Foot Ankle Int. 2020 Oct;41(10):1271-1276.
Houck J, et al. Randomized Controlled Trial Comparing Orthosis Augmented by Either Stretching or Stretching and Strengthening for Stage II Tibialis Posterior Tendon Dysfunction. Foot Ankle Int. 2015 Sep;36(9):1006-16.
Durrant B, et al. Posterior tibial tendon dysfunction: a review. J Am Podiatr Med Assoc. 2011 Mar-Apr;101(2):176-86.
Geideman WM, Johnson JE. Posterior tibial tendon dysfunction. J Orthop Sports Phys Ther. 2000 Feb;30(2):68-77.
Ross MH, Smith MD, Mellor R, et al. Exercise for posterior tibial tendon dysfunction: a systematic review of randomised clinical trials and clinical guidelines. BMJ Open Sport & Exercise Medicine 2018;4:e000430.
Gómez-Jurado I, Juárez-Jiménez JM, Munuera-Martínez PV. Orthotic treatment for stage I and II posterior tibial tendon dysfunction (flat foot): A systematic review. Clin Rehabil. 2021 Feb;35(2):159-168.