Constipation can oftentimes be difficult to discuss, even with a health professional. It is a defecation disorder that can significantly impact daily life and should not be neglected. Normal bowel movements occur up to 3 times per day or 1 to every 3 days. If your bowel movements occur less than twice per week, continue reading.
Defining constipation
Constipation is defined by the International Urogynecological association as “a complaint that bowel movements are infrequent and / or incomplete and/or there is a need for frequent straining or manual assistance to defecate”. Infrequent bowel movements occur twice per week, the rectum does not feel empty after opening the bowels. The final criterium is excess effort or manual assistance to assist with evacuation.
Constipation can occur spasmodically in response to travel, lifestyle changes, activity levels, diet and hormonal profile, this is called occasional constipation. Chronic constipation differs to occasional constipation with symptoms presenting for more than 25% of bowel movements for at least 6 months. Clinically, the Rome Criteria assists with the diagnosis of functional constipation in the presence of two or more of the following symptoms:
- Straining during more than ¼ (25%) of defecations
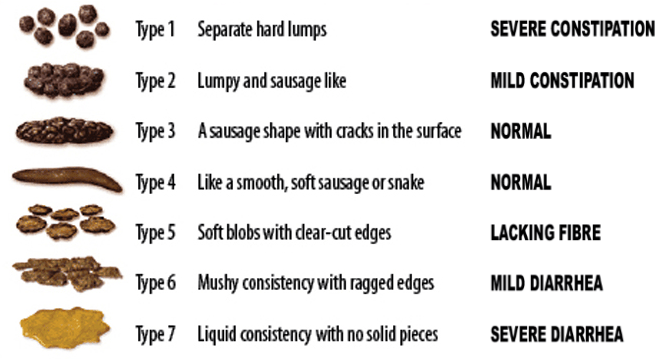
- Lumpy or hard stools (Bristol Stool Form Scale 1-2) more than ¼ (25%) of defecations
- Sensation of incomplete evacuation more than ¼ (25%) of defecations
- Sensation of anorectal obstruction/blockage more than ¼ (25%) of defecations
- Manual manoeuvres to facilitate more than ¼ (25%) of defecations (e.g., digital evacuation, support of the pelvic floor)
- Fewer than three soft bowel movements per week
- Loose stools are rarely present without the use of laxatives
- Insufficient criteria for irritable bowel syndrome
The Bristol Stool Scale provides a clinical guide for the type of bowel movement.
Types of constipation
There are 2 subtypes of constipation, which we can think of in the context of processing and evacuation to simplify things.
1) Slow transit constipation
Slow transit constipation occurs when the journey from the colon to the rectum is delayed. Normal colonic transit time is between 25 and 40 hours. Over 48 hours will result in increased water absorption and a firmer stool and an infrequent desire to defecate. Clinically, clients present with infrequent and hard stools.
2) Obstructed defecation
As it appears, obstructed defecation means there is difficulty evacuating the stool from the rectum via the anal canal. There are no issues with the colonic transit time it is the result of a pelvic floor dysfunction. Pelvic floor dysfunction can be broken into two types:
- Dyssynergic defecation: one of the pelvic floor muscles contracts and creates a kink in the anal canal disabling release.
- Structural obstruction: prolapse of the vaginal wall or the rectum.
Obstructed defecation will result in the feeling of incomplete bowel movements, straining or the sensation of a blockage.
Possible causes
- Cancer or cancer related causes
- Hormonal changes
- Metabolic disorders
- Gastrointestinal disorders
- Neurological conditions
- Psychological conditions
- Pregnancy
- Age
- Medications
- Other factors such a sexual trauma, privacy and time
Engaging with a General Practitioner will guide the treatment pathway and rule out alternative diagnoses. This will involve an anorectal exam whereby your Physician will visually and digitally assess the rectum for masses, strictures, blockages and tone. This may be accompanied by an X-ray. Your Physician will review your medication list for any possible contributing pharmacological agents that can be altered to another type, dosage or key ingredient.
Management strategies
Unfortunately, there is not a lot of evidential support for lifestyle intervention regarding constipation however it is the least invasive and requires little effort to implement changes. Being aware of the signals to pass a bowel movement is a great starting point, this will usually occur after a meal and if ignored, can reduce normal rectal signalling overtime.
Increasing fluid and fibre intake are commonly recommended for the management of constipation. Water intake for healthy adults should be 1.5-2 litres. Evidence shows that increasing water consumption above this recommended amount will not reduce constipation however drinking less than 500ml will reduce bowel movement frequency. Studies have validated increases in both fluid intake frequency and fibre ingestion as a combined therapy. In the pregnant population, increasing fluid intake has demonstrated positive effect on pregnancy related constipation.
Recommended fibre intake is between 20-35 grams for healthy adults. Fibre can be found in fruits, vegetables, nuts, legumes, breads, pastas and cereals. Alternatively, fibre supplementation, laxatives, caffeine and exercise can aid constipation. Laxatives and other fibre supplements when used in excess can cause diarrhoea and abdominal discomfort.
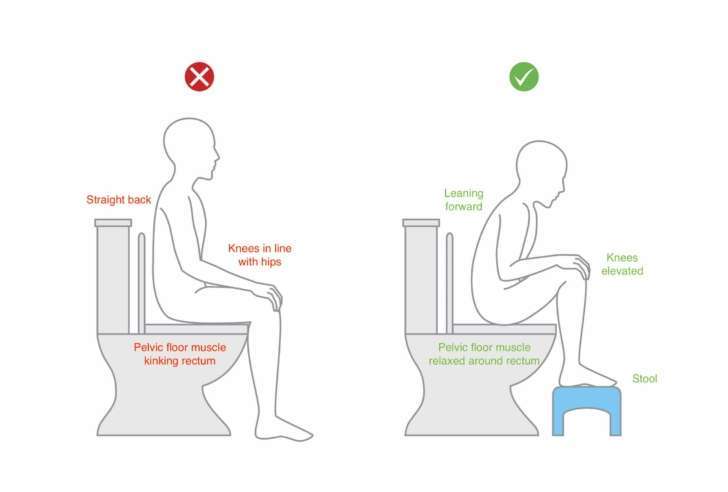
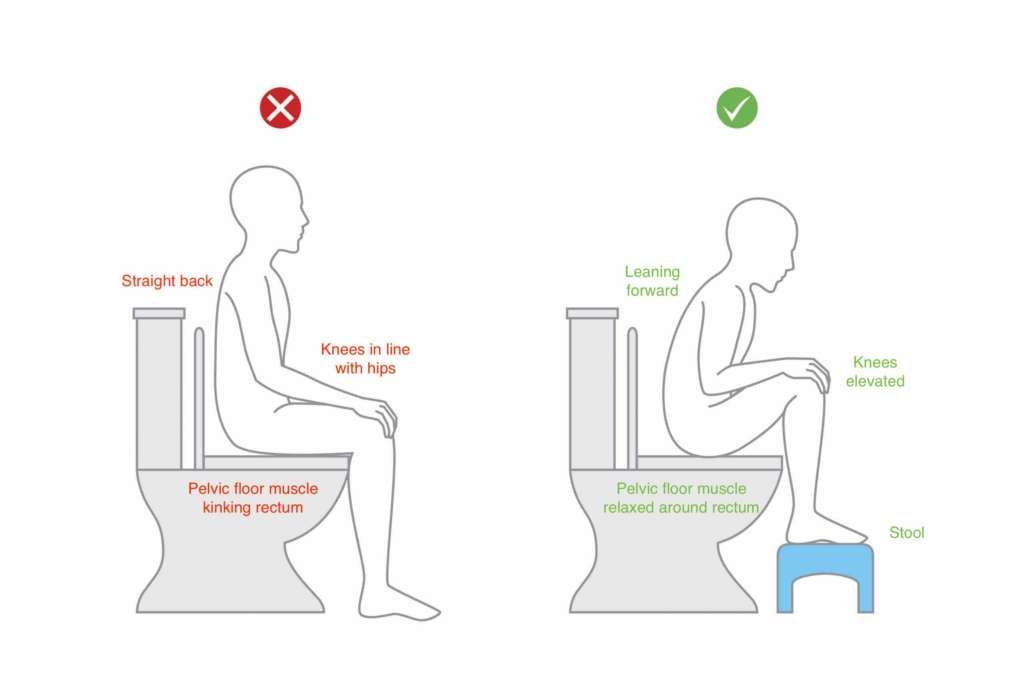
Toileting posture and position
Ensuring correct posture and position when opening the bowels is vital to reduce strain on the pelvic floor, reduce dyssynergic motor control and allow for complete emptying. When opening the bowels:
- Lean forward with your trunk
- Rest the elbows onto the knees
- Ensure the knees are above the level of the hip
- Use a stool or toilet roles to elevate the feet – DO NOT go onto the tip toes
Breathe, brace and bulge technique:
- Breathe into the belly and relax the shoulder and upper body, this is also called diaphragmatic breath.
- Brace the stomach by trying to widen the waist. With your hands on your waist, try and move your ribs down and out. As if you are pretending to blow up a balloon without breathing out.
- Bulge your stomach outwardly
- Maintain the breath, and push into the belly and waist a little more to bring the bowel movement into the rectum
- Once you have passed the bowel movement, contract/ lift the pelvic floor to ensure complete closure. Imagine picking up a blueberry with your back passage.
Ensure that you are not holding the breath when toileting, bearing down or straining to pass a bowel movement. See diagram below for guidance.
References:
- Schuster BG, Kosar L, Kamrul R. Constipation in older adults: stepwise approach to keep things moving. Can Fam Physician. 2015 Feb;61(2):152-8.
- Chung BD, Parekh U, Sellin JH. Effect of increased fluid intake on stool output in normal healthy volunteers. J Clin Gastroenterol. 1999 Jan;28(1):29-32.
- Anti M, Pignataro G, Armuzzi A, Valenti A, Iascone E, Marmo R, et al. Water supplementation enhances the effect of high-fiber diet on stool frequency and laxative consumption in adult patients with functional constipation. Hepatogastroenterology. 1998 May-Jun;45(21):727-32.
- Effective techniques for opening bowel. Anorectal Physiology/GI Physiology, July 2020.