The shoulder is an especially complex area of the body, anatomically speaking, and unfortunately that means there are many potential areas for injury. The shoulder joint encompasses the junction where the upper arm bone (humerus) meets the collar bone (clavicle) and the shoulder blade (scapula) at the back.
The ligaments of the shoulder are relatively weak and therefore the joint relies on the surrounding muscles for stability, specifically a group of muscles known as the Rotator Cuff. These muscles maintain the “ball” of the humerus in the socket of the joint. The rotator cuff muscles play an essential role in shoulder movement and therefore are often involved in shoulder injuries, but there are many other structures, such as cartilage, tendons, labrum, bursa and nerve roots, which can also be affected.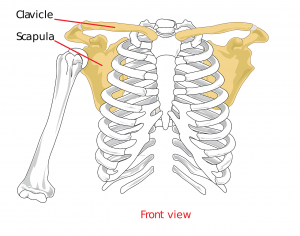
Shoulder injuries frequently present after a gradual onset, often in the dominant arm due to overuse, e.g. persistent work posture or an athlete who uses a dominant arm repetitively (e.g., to throw). However, shoulder injuries can also be caused by a sudden impact, as is often the case with dislocations.
While there are many conditions that can affect the shoulder, these are five common ones that we see commonly in our Newcastle physiotherapy clinic.
1) Rotator cuff tears
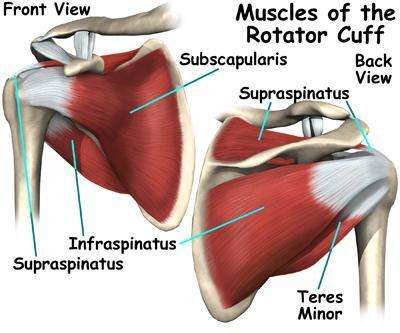
Four muscles make up the rotator cuff of the shoulder:
- Supraspinatus
- Infraspinatus
- Subscapularis
- Teres minor
The tendons of these muscles criss-cross the shoulder joint, closely passing over the joint capsule, resulting in them being prone to tears either in the tendon or the muscle itself. The tendon of the long head of the biceps muscle can also be involved as it connects to the top of the shoulder joint. Advanced age is a predisposing factor to rotator cuff tears, as tendons calcify and become less elastic due to wear and tear. Another aggravating factor can be repetitive overhead activity, e.g., painting or construction work. Symptoms may include a dull, deep ache and restriction of movement when reaching overhead or behind the back.
Management of the injury will depend on the severity of the tear. Initially, the priority is resolving inflammation with rest, ice and then physiotherapy. Eventually treatment should address strengthening of the muscle; however premature strengthening may delay healing and cause further problems. Severe tears may require surgical repair, but in most cases physiotherapy is the first course of treatment.
2) Cervical radiculopathy
Sometimes pain in the shoulder doesn’t originate from the shoulder at all. Cervical radiculopathy is the medical term for a “pinched nerve” in the neck. The nerves that supply the entire shoulder and arm branch out from the spinal column in the neck, meaning that if a certain area is injured or inflamed, it can cause referred pain into the shoulder. The nerves can be encroached upon by a bulging intervertebral disc, chemical irritants from swelling and inflammation, or simply tight muscles. Overactive muscles can tighten, shorten and form “knots”, resulting in referred pain. Neck issues can also produce weakness and/or tingling in the shoulder and arm, usually a reliable sign that a nerve is involved.
Treatment initially should be aimed at pain relief and the management of inflammation. Once pain settles, normal range of movement should be restored, with a focus on posture correction, movement control training, strengthening and finally trying to prevent a recurrence.
3) Shoulder impingement
Shoulder movement should naturally occur in a smooth and pain-free pattern; however, sometimes the rotator cuff tendons become trapped and inflamed, resulting in what is known as impingement. If this continues over an extended period of time, it can cause rotator cuff tendonitis or shoulder bursitis.
Impingement is most commonly seen in athletes who perform repetitive overhead actions, e.g. swimmers, tennis players, cricket fast bowlers, etc., or in occupations such as construction and painting where workers are repeatedly reaching overhead for prolonged periods of time.
Impingement can also occur secondary to dynamic instability in the shoulder, where weak muscles and lax ligaments result in excessive movement of the shoulder joint. In this situation, the rotator cuff muscles work overtime to stabilise the joint, causing fatigue and overuse injuries.
Arthritis may also be a contributing factor in older populations, as it can cause a narrowing of the joint space resulting in impingement.
Shoulder impingement usually presents as pain radiating down the side of the arm, starting as a niggle but worsening if no action is taken. Treatment should focus on pain relief and symptom management, movement retraining and then strengthening once the symptoms have eased. Corticosteroid injections can also be helpful in the initial anti-inflammatory stages if more conservative techniques are unsuccessful.
4) Shoulder dislocation and shoulder instability
The shoulder is the body’s most mobile joint and therefore prone to dislocation, where the joint “pops out” of place. Shoulder dislocations are a common occurrence in many sports, especially rugby due to the impact of tackles, but also AFL as players take marks with arms overhead and the joint in a vulnerable position.
Unfortunately, it is common for patients to experience recurrent dislocations, resulting in serious joint instability and oftentimes in secondary impingement, as mentioned above. The shoulder joint can dislocate in various directions and cause damage to the surrounding structures, which makes rehabilitation additionally complex.
To prevent future dislocations, the rotator cuff muscles must be strengthened in all ranges of movement to help stabilise the joint in various positions. Strapping and bracing techniques are also used to provide extra stability, particularly if returning to sport. Surgery may be necessary depending on the severity of the dislocation, but expert physiotherapy treatment will be essential regardless.
5) Frozen shoulder
Frozen shoulder is the common term for adhesive capsulitis, which presents as pain and stiffness in the shoulder, and can sometimes be confused for a rotator cuff injury. It seems to be caused by inflammation of the joint capsule and, while it is unknown what starts the inflammatory process, certain medical conditions such as diabetes, hypothyroidism, hyperthyroidism and cardiac disease are linked with an increased risk of developing frozen shoulder.
A true frozen shoulder has three distinct phases which can each take up to six months to pass
- Freezing/inflammatory stage – characterised by pain and then a progressive loss of range of movement. Aggressive treatment should be avoided in this phase to prevent further inflammation and the main treatment goal should be pain management and prevention of loss of movement.
- Adhesive/frozen stage – pain usually resolves towards the end of this phase, however stiffness persists.
- Thawing stage – gradual return of normal range of movement, this is the phase when manual therapy can have its greatest effect.
Frozen shoulder is a extremely frustrating condition and requires immense patience. The goal of physiotherapy is to maintain and then regain as much range of movement and muscle strength as possible. There is no quick fix, but physiotherapists can guide you through the recovery process to ensure you recuperate as rapidly as you can.
A medical procedure known as hydrodilation is sometimes used in conjunction with physiotherapy. This involves local anaesthetic, saline and cortisone being injected into the shoulder joint to stretch the capsule and break down any adhesions. It is currently not known whether this procedure enhances recovery compared to physiotherapy alone, but it may be an option worth discussing with your treating doctor.
Shoulder rehabilitation techniques
Pain
The first step with any injury is to manage pain and inflammation. This may be achieved through resting the joint, unloading affected muscles or sometimes even immobilising the shoulder. Care should be taken to prevent muscle wasting, and not to neglect adjacent joints, keeping the elbow, wrist and hand moving and functioning with full strength. If the shoulder joint needs to be immobilised, then your physiotherapist will be able to prescribe appropriate gentle exercises to prevent stiffness.
Posture
Once pain is under control, posture needs to be addressed, as it is often a contributing factor to shoulder conditions. It sounds like an easy fix, however breaking bad habits can take time. The important thing is to implement a good routine so that correct posture becomes automatic.
One of the main areas of posture that should be assessed is scapular stabilisation. The correct scapular position is rotated downwards and back; a common mistake patients make is sticking the chest out, however it is better to think of keeping your shoulders “back and down.” By using the muscles of your upper back to draw the shoulder blades into correct position, you can reduce the load on the often-overactive neck musculature.
People often focus on their neck, back and shoulders when trying to improve their posture, however sometimes the culprit can be on the front of their chest instead. The pectoral muscles (often called the pecs) lie across the front of the chest and when tight can rotate the shoulders, creating a slouched posture. This is most commonly seen in desk workers, but also sometimes in those who do strength training at the gym. These people may focus on the pectorals for aesthetic reasons, but neglect the mobility and strength of their back muscles which causes an imbalance.
Work station set up
Anyone who spends a significant time working at a computer should undertake a complete ergonomic assessment.
Consider the following basic points:
- Is the monitor at the correct height?
- Is the chair in correct position for legs and lumbar support?
- Are your arms at an appropriate height relative to your desk?
- Are the keyboard, mouse and phone hand-set at an appropriate distance?
A poor ergonomic set up results in having to twist or reach throughout the day, which if done many times can quickly lead to shoulder pain and poor postural adaptations.
It is beneficial to complete quick, gentle shoulder and neck stretches at regular intervals during the day. Have a post-it note next to your desk reminding you to do your stretches and check your posture. The same applies for people who use a laptop, even if it’s only at home doing online shopping or watching Netflix, be mindful of your posture. Believe it or not, slumping on the couch is a very common cause of neck and shoulder problems.
If you have concerns about your ergonomics, your physiotherapist will be able to conduct a formal ergonomic assessment at your office to give you expert advice and equipment recommendations (if any).
Taping
Strapping tape can sometimes be used either to give support to an unstable shoulder or facilitate correct posture. By taping a shoulder into the correct place, you are reminded during the day how it should be positioned. Taping is not a permanent fix though, as the muscles need to start doing their job properly on their own. Another taping method is to offload overactive muscles inhibiting their use. Taping should only be trialled initially by a physiotherapist to ensure correct positioning and effectiveness. The physio can then sometimes teach a patient how to self-tape, if required.
Range of movement
The shoulder moves in several planes and for full function all of the muscles and ligaments need to be working together. Stiffness and pain can negatively impact the range of motion so active movement and passive stretching may be required to regain full movement. There are many specific techniques that your physiotherapist may use. As an example, gentle mobility exercises can be done holding a broomstick handle moving the joint through its full range, both in a forward and sideways direction.
Strengthening
Once the shoulder is moving in alignment and with the correct muscle patterning, strengthening can commence. It is usually required to begin with very simple exercises, before progressing to strengthening the joint while moving.
Strengthening should address all of the muscles which stabilise the shoulder blade and the move the upper arm. It is beneficial to strengthen the muscles in many different positions and through various ranges of movement.
Massage
A very popular method of pain relief, massage may be effective at releasing tight muscles and knots, which can allow you to focus on your rehabilitation exercises more easily. Massage is a fantastic tool, but keep in mind that it does not correct poor posture, movement patterns, or the underlying anatomy. It is best used in conjunction with physiotherapy prescribed exercises to prevent the recurrence of the muscle tension and pain.
Surgical intervention
Procedures such as steroid injections or nerve blocks have their place in managing some injuries, however, these interventions are generally only used in very specific conditions and always alongside physiotherapy treatment.
Surgery should always be the last resort for any injury and only explored once all other routes have been unsuccessful. Surgery is in no way a quick fix as the shoulder will never be 100% again due to scar tissue and change of intrinsic anatomy. Scar tissue develops as a defence mechanism to protect an area therefore it is not as flexible as natural tissue. Many procedures require the joint to be immobilised for a period post-operatively to allow for healing. This causes stiffness and muscle weakness which then requires physiotherapy rehabilitation to resolve.
Shoulder surgery can include:
- Arthroscopy – keyhole surgery where a camera is inserted into the joint and it can be cleaned up of scar tissue and adhesions
- Arthroplasty – a full joint replacement
- Mobilisation under anaesthesia – manipulation of the joint while the patient is asleep to break through any restrictions
In most cases, your surgeon will advise that you seek physiotherapy treatment both before (pre-habilitation) and after (rehabilitation) surgery.
See A Physiotherapist
As always, any injury should be assessed thoroughly by a physiotherapist who will then prescribe treatment based on their findings. Every case is unique, so make sure you seek professional and personalised advice.
If you have a shoulder complaint and want to get expert guidance, book in with one of our clinicians at Peak Physio in Newcastle today.